- If cause of hyponatremia is rapidly reversible - If cause of hyponatremia is unlikely to be rapidly reversible. A fluid restricted diet helps prevent fluid from building up in the body.
Tips To Assess Rapid Onset Of Hyponatremia To Prevent Overcorrection And Diagnose Underlying Cause Acep Now from www.acepnow.com
The two groups also differed in etiology of SIAD - more patients in the fluid restriction group had respiratory disease 5 vs 3 and idiopathic SIAD 9 vs 6 while fewer had CNS pathology 0 vs 3.
Fluid restriction for hyponatremia. An Effective and Practical Fluid Restriction Protocol to Decrease the Risk of Hyponatremia and Readmissions After Transsphenoidal Surgery. The implementation of 1000-mL fluid restriction between POD 4 and 8 is a highly successful and simple approach to decrease the risk of delayed hyponatremia after TSS. The implementation of 1000-mL fluid restriction between POD 4 and 8 is a highly successful and simple approach to decrease the risk of delayed hyponatremia after TSS.
33 rows In general hyponatremia is treated with fluid restriction in the setting of. A restriction of 1 liter or 15 liters will be inadequate Patients and families might worry that fluid restriction will cause dehydration Dr. Stressing that hypo-osmolar hyponatremia is a condition of too much wateror water intoxicationmay help patients and families accept that water restriction is appropriate.
Fluid and salt restriction Consider diuretics Treat the underlying cause Euvolaemic hyponatraemia If possible treat the cause eg. Chest infection malignancy or hormonal insufficiency If treating SIADHAppendix 3- Commence fluid restriction 500 -750 mlday Maintain accurate fluid balance chart. Water excretion is normal in these patients and water restriction corrects the hyponatremia.
In a patient on a normal diet and an average solute protein and salts intake a substantial amount of. SIADH Fluid Restriction Can calculate if treatment will be successful. Una Uk Sna Sk 1 unlikely will be successful with fluid restriction 05 1 likely will be successful with 500 cc fluid restriction 05 likely will be successful with 1 L fluid restriction.
- If cause of hyponatremia is rapidly reversible - If cause of hyponatremia is unlikely to be rapidly reversible. Additional measures in all patients. SUBSEQUENT THERAPY FIRST SEVERAL DAYS Monitoring.
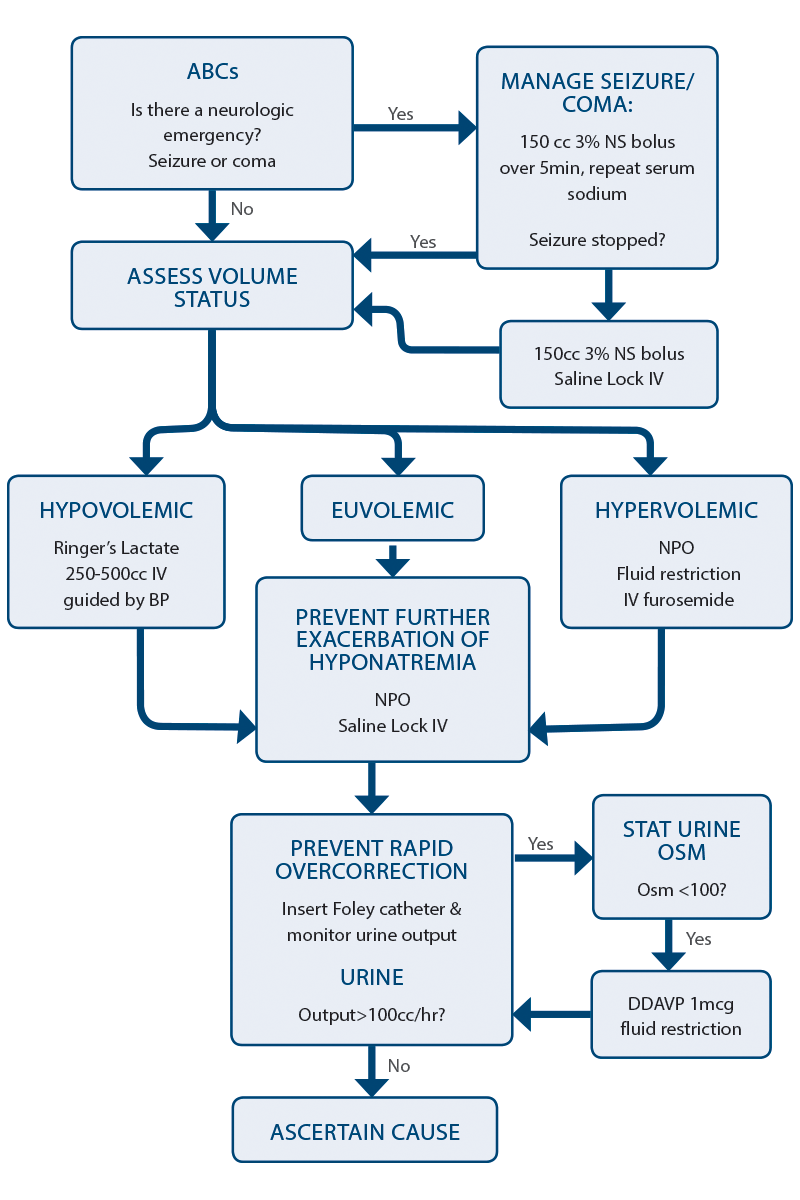
Subsequent therapy of chronic hyponatremia - Discontinuing hypertonic saline used as initial therapy - Fluid restriction. Overly rapid correction particularly in chronic hyponatremia can lead to osmotic demylination syndrome ODS previously known as central pontine myelinolysis CPM. In most cases sodium correction should be done in an ICU setting especially with hypertonic fluids for replacement.
On univariate analysis hyponatremic babies had a greater net positive fluid balance 749 vs 1147 mLkg p 0001 primarily due to a decrease in total fluid output p 005. On multivariable regression a 10 mLkg increase in overall fluid balance was associated with an increased risk of developing hyponatremia OR 184 123 345 p 0016. The fluid restriction was changed to 1 literday 12 litersday if weight 100 kg EXP 2 n18 during the study due to interim analysis suggesting a trend toward a reduction in the incidence of hypoNa with fluid restriction.
Patients in the CON group were instructed to drink ad lib. Water restriction Traditionally fluid restriction 115 Ld has been considered the first-line option for treating hyponatremia associated with cirrhosis. To be effective fluid intake has to be limited to 500 ccd below the combined 24-hour urine output and insensible losses 5.
The goal is to achieve a state of negative water balance. The Fluid restriction group had a mean duration of hyponatremia of 19 months whereas the No Treatment group had 71 months mean duration. The two groups also differed in etiology of SIAD - more patients in the fluid restriction group had respiratory disease 5 vs 3 and idiopathic SIAD 9 vs 6 while fewer had CNS pathology 0 vs 3.
All patients should be placed on fluid restriction including all oral and intravenous fluids of 1 Lday. This should be adjusted based on measured urine output and set at 500 mL less than daily urine volume eg a patient producing 1200 mLday of urine should be placed on 700 mLday fluid restriction. Pending further study to avoid hyponatremia and to decrease the risk of complications associated with excessive fluid administration we suggest.
Literature describes syndrome of inappropriate anti diuretic hormone SIADH as the mechanism of hyponatremia in COVID-19 requiring fluid restriction for management. However it is important to rule out other etiologies of hyponatremia in such cases keeping in mind the effect of an alternate etiology on patient management and outcome. Fluid Restricted Diet.
A fluid restricted diet limits the amount of fluid you consume each day. In addition to beverages many foods provide fluids. Examples include ice cream yogurt gelatin pudding soups sauces and juicy fruits.
A fluid restricted diet helps prevent fluid from building up in the body. Fluid restriction should be the main stay of treatment for all other causes of hyponatremia. The rate of correction of hyponatremia should generally be a rise of 6-9mmolL24 hours but never exceed 12mmolL24 hours due to the risk of sudden osmotic shift and demyelination.
If a person take 650 mOsm daily one can drink up-to 65050 minimal urine osmolarity ie. Maximal free water excretion 13 L of water without causing hyponatremia. If a person has potomania beer drinkers hyponatremia only intake about 200 mOsm daily.
Any water intake 20050 4L will cause hyponatremia.