An example of a nurse demonstrating this ethical principle is by holding a dying patients hand. An example of a nurse demonstrating this ethical principle is by holding a dying patients hand.
The principle of beneficence underscores the moral obligation to act for the benefit of others here patients including protecting the rights of others preventing harm to others and helping those in danger1 One can see that respect for autonomy and beneficence may at times be in conflict such as when a competent patient refuses a.
Example of beneficence in medical ethics. Keep on top of the hot topics that you can apply the principle of beneficence for example. Charlie Gard how did Doctors consider beneficence. Vaccinations can HPV vaccinations be justified as mandatory on the grounds of beneficence.
Abortion how does beneficence factor here. Hearing about medical or nursing ethics in the health care field is as easy as listening to the radio or turning on the news. 1 Beneficence involves the moral imperative of.
More commonly in medical ethics beneficence is understood as a principle requiring that physicians provide and to the best of their ability positive benefits such as good health prevent and remove harmful conditions from patients. This is to say that beneficence as a principle of medical ethics asserts an obligation on the part of the. According to Charlesworth 2001 the principles of medical ethics are shared by other branches in the area of health care and a good example is the nursing ethics.
Among the principles used in medical ethics is the beneficence and the nonmaleficence principle. Dont use plagiarized sources. Get Your Custom Essay on.
According to the AOTAs Code of Ethics and Ethics Standards 18 examples of application of beneficence include demonstrating concern for the well-being of those receiving OT services through referral to other health-care professionals when appropriate and providing current assessment and intervention. 18 A specific example of application of this principle to gerontological practice would be. Ception of beneficence still dominant in the minds of many physicians and patients.
It still shapes the ethos and ethics of medicine. It is the conception too that is the focus of criticism by the proponents of autonomy who equate beneficence almost entirely with medical paternalism. For example the notion that the physician ought not to harm any patient is on its face convincing to most people.
Or the idea that the physician should develop a care plan designed to provide the most benefit to the patient in terms of other competing alternatives seems both rational and self-evident. One of the best ways to understand the difference between non-maleficence and beneficence is by looking at an ethical example. A 52-year-old man collapses in the street complaining of severe acute pain in his right abdomen.
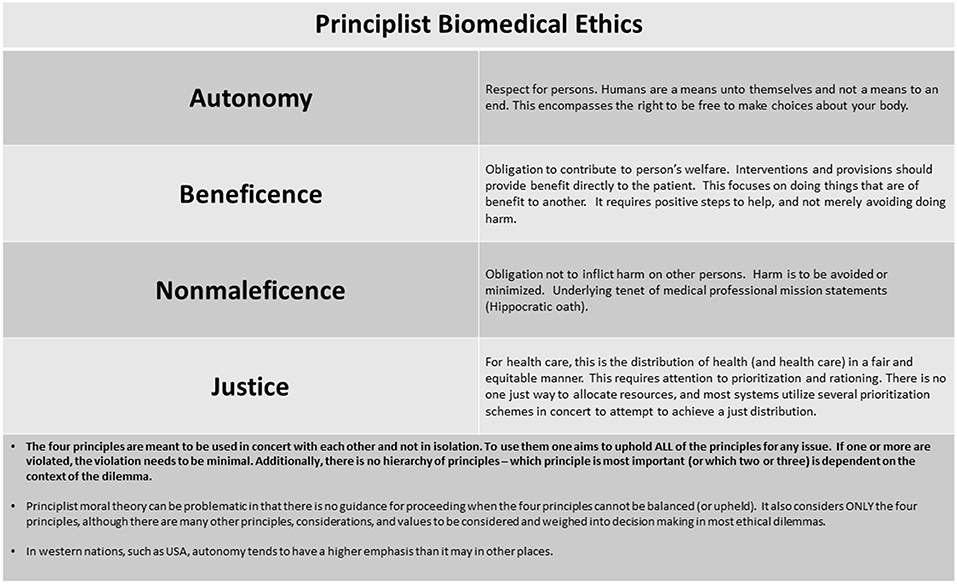
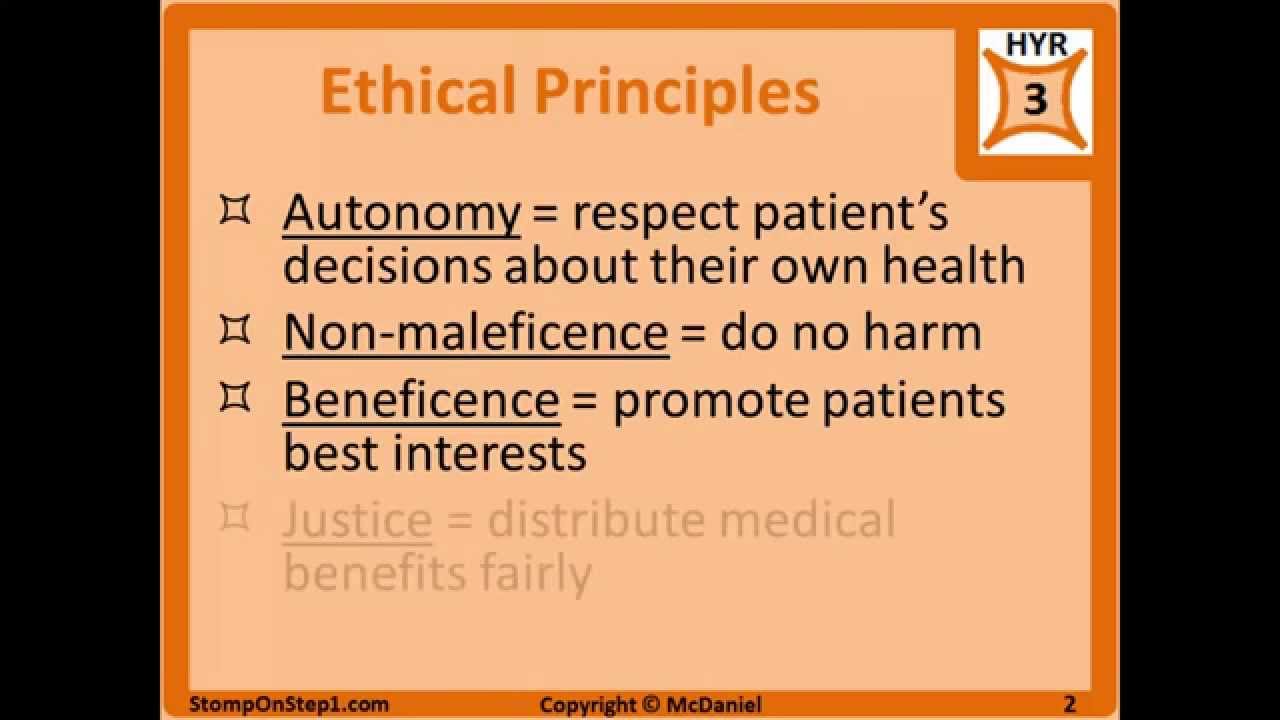
A surgeon happens to be passing and examines the man suspecting that he is on the brink of rupturing his appendix. The four basic pillars of medical ethics are beneficence non-maleficence justice and autonomy 4. At a glance these principles appear simple and there are many examples of clearly unethical medical decisions.
Yet ethical dilemmas are common within medicine and there is not always an agreed-upon right decision. The principle of beneficence underscores the moral obligation to act for the benefit of others here patients including protecting the rights of others preventing harm to others and helping those in danger1 One can see that respect for autonomy and beneficence may at times be in conflict such as when a competent patient refuses a. Ethics is an understanding of the nature of conflicts arising from moral imperatives and how best we may deal with them.
Ethics in medical research deals wit. The following are a few examples the UCSF provides in regard to beneficence. Resuscitating a drowning victim providing vaccinations for the general population or helping someone quit smoking Pantilat 2008.
Ethics in medical research deals with the conflicts of interest across various levels. Guidelines have been proposed for standardized ethical practice throughout the globe. The four fundamental principles of ethics which are being underscored are autonomy non-maleficence beneficence and justice.
Beneficence is defined as kindness and charity which requires action on the part of the nurse to benefit others. An example of a nurse demonstrating this ethical principle is by holding a dying patients hand. Justice means being impartial and fair.
Double effect refers to two types of consequences that may be produced by a single action and in medical ethics it is usually regarded as the combined effect of beneficence and non-maleficence. A commonly cited example of this phenomenon is the use of morphine or other analgesic. Respecting the principles of beneficence and non-maleficence may in certain circumstances mean failing to respect a persons autonomy ie.
Respecting their views about a particular treatment. For example it may be necessary to provide treatment that is not desired in order to prevent the development of a future more serious health problem.