The relationship between Rheumatoid Arthritis and prevalence. If anti-HP IgM and IgA or IgG were positive the case was considered related to HP.
His diarrhoea resolved over 7 days.
Can h pylori cause rheumatoid arthritis. So I highly encourage you to Eradicate H Pylori in a bid to improve your Rheumatoid Arthritis however I seriously doubt that such a measure ALONE will put you into remission. If you wish to seek to be in remission then youll need to go all in and do a program such as the Wahls Protocol that will give you an entire framework from which to reverse your autoimmune disease. Rheumatoid arthritis RA is an autoinflammatory disease caused by genetic susceptibility and environmental triggers which include infectious agents.
Helicobacter pylori a bacterium that frequently colonizes the stomach is associated with the development of certain autoinflammatory disorders. This study examined a possible association between H. Our data suggest that H.
Pylori infection is implicated in the pathogenesis of rheumatoid arthritis in that its eradication may induce a significant improvement of disease activity over 24 months. Pylori eradication seems to be advantageous in infected rheumatoid arthritis patients but controlled studies are needed. The frequency and relationship between H.
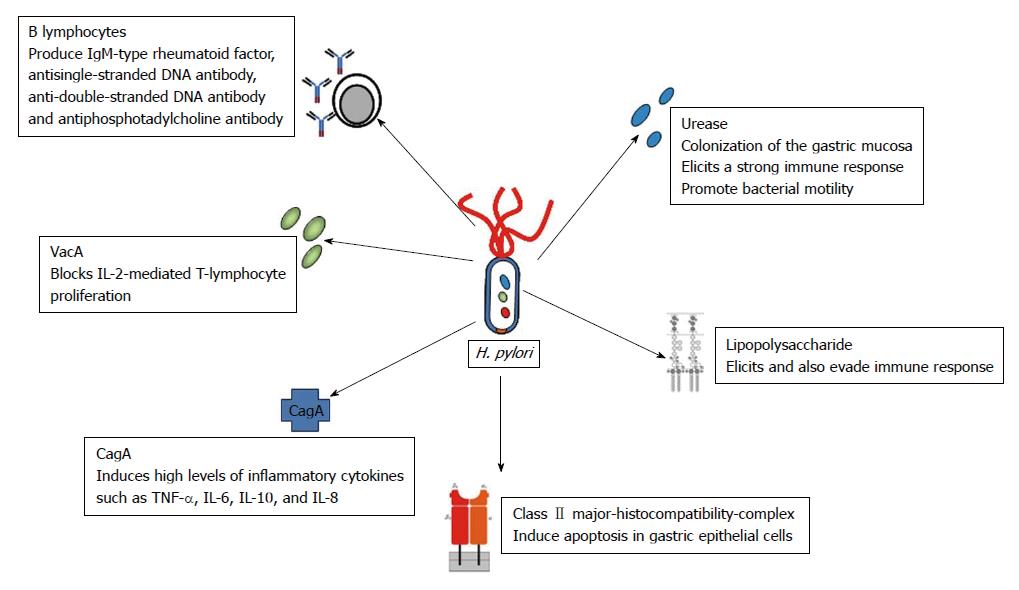
Pylori infection and systemic lupus erythematosus rheumatoid arthritis autoimmune atrophy gastritis and autoimmune pancreatitis were evaluated using the data from 43 studies involving 5052 patients. According to statistical analysis it is probable that infection with more virulent strains of H. Pylori such as H.
Pylori cagA positive can increase the risk. Hp infection has been associated with digestive diseases and rheumatic diseases 1. It remains unclear whether all or part patients of rheumatic diseases should be routinely screened for Hp infection.
We have examined predictors of Hp infection in rheumatic diseases so as to define who might benefit most from screening. Four cases of reactive arthritis ReA related to Helicobacter pylori HP are presented. These were identified by IgG IgM and IgA ELISA tests performed on sera obtained from a 2-year prospective study on 186 patients with a clinical picture suggesting ReA as a possible diagnosis.
If anti-HP IgM and IgA or IgG were positive the case was considered related to HP. Three out of four HP ReA. Infection with H.
Pylori had no significant effect on RA pathogenesis especially since the prevalence of rheumatoid arthritis in countries with high rates of colonization with H. 91 94 95 In the recent years atrophic gastritis has been classified into multifocal caused by H. Pylori and autoimmune atrophy gastritis.
Helicobacter pylori H. Pylori is a widely prevalent microbe with between 50 and 80 of the population infected worldwide. Clinically infection with H.
Pylori is commonly associated with peptic ulcer disease but many of those infected remain asymptomatic. Pylori has evolved a number of. The relationship between Rheumatoid Arthritis and prevalence.
And tested for Rapid Hpylori and CMV IgG all RA patients were also tested for quantitative RA IgG IgM and IgA. The results showed an elevated concentrations of RA IgG IgM and IgA compared to the normal value of less than 20 Uml results also showed no significance differences in the percentage of positive result. Helicobacter pylori H.
Pylori infection has been reported to be associated with various diseases including arthritis. Pylori may ameliorate disease activity of rheumatoid arthritis RA whereas reactive arthritis after successful H. Pylori eradication has been reported.
Eradication of Helicobacter pylori infection appears to reduce the severity of rheumatoid arthritis. This suggests that H pylori infection plays a role in the pathogenesis of rheumatoid arthritis. An infectious agent has been previously postulated as a triggering agent for rheumatoid arthritis explain investigators from the Universita di Genova in Genoa Italy.
The investigators set out to. Helicobacter pylori and nonsteroidal antiinflammatory drugs NSAIDs are considered the major causes of peptic ulcer. If ulcers are not attributable to H.
Pylori most are thought to be attributable to NSAIDs. We have previously reported that rheumatoid arthritis RA patients taking NSAIDs long term NSAIDs group are more likely to develop gastric ulcers which commonly occur in the gastric. Rheumatoid arthritis is an inflammatory chronic disease with an autoimmune pathogenesis.
To determine the role of Helicobacter pylori as a trigger agent twenty five patients with rheumatoid. He was treated with sulfazalazine celecoxib and metronidazole. His diarrhoea resolved over 7 days.
His arthritis persisted and required intra-articular administration of corticosteroids to his right ankle. There was slight improvement in his arthritis in the next 3 months but he was unable to return to work. There was no evidence of development of a systemic rheumatologic disease during this time.
Pylori is suspected to be one of the factors triggering rheumatoid arthritis. The aim of this study was to evaluate the effect of H. Pylori eradication on inflammatory disease activity in patients with rheumatoid arthritis.
I read that H pylori lowers stomach acid which leads to increased calcum levels in the blood and degenarative diseases calcification and bone spurs. Pylori infections can also lead to iron-deficiency anemia. I am 35 years old woman.
I tried antibiotics to treat H pylori but that did not help and caused yeast infections.